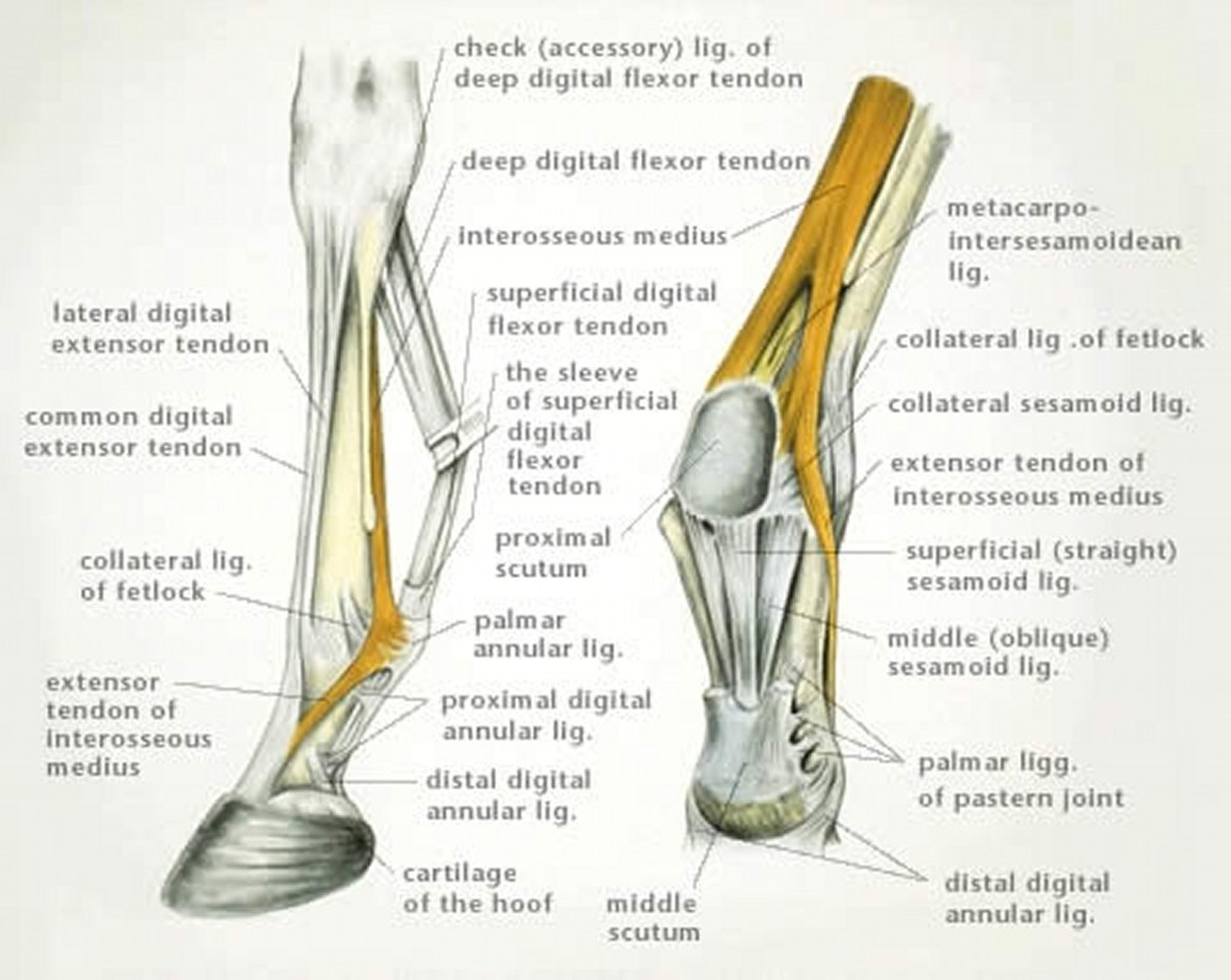
Illustration by Dr. Gheorghe Constantinescu
Injuries of the suspensory ligament (interosseous muscle) are common in forelimbs and hindlimbs of horses. Lesions are typically classified as affecting the proximal, body, or branches of the suspensory ligament.
Proximal Suspensory Desmitis:
The term proximal suspensory desmitis (PSD) is restricted to lesions confined to the proximal one-third of the metacarpus. PSD can occur unilaterally or bilaterally and is a common injury in all types of athletic horses. Injury to the proximal suspensory ligament and/or its attachment to the proximal palmar aspect of the third metacarpal bone typically results in sudden onset lameness that seems to improve within a few days. Lameness varies from mild to moderate and is typically not severe unless there is substantial involvement of the ligament and its attachment (avulsion of the palmar cortex). If the horse has bilateral PSD, there may be less overt lameness but more loss of action of the horse. Lameness is typically more noticeable on soft ground and with the affected leg on the outside of the circle. Response to distal limb and/or carpal flexion tests is variable. Pressure applied to the proximal palmar metacarpal region may elicit pain; however, this response/reaction should be compared with that of the other limb to determine significance.
Diagnosis of PSD usually requires localization with diagnostic analgesia, because typically horses do not have clinical signs (eg, heat, pain, swelling) that allow lameness to be localized to this region. There are multiple techniques to desensitize the proximal aspect of the palmar metacarpus. However, there is confusion interpreting the results of subcarpal analgesia because of the lack of specificity of local analgesic techniques. After lameness has been localized, radiographs as well as ultrasonographic examination of the region should be performed. Ultrasound of the proximal suspensory should be critically compared with that of the other limb, remembering that bilateral lesions do exist. Nuclear scintigraphy can help detect osseous injury at the proximal suspensory attachment, but negative scintigraphic images do not exclude the presence of PSD. MRI is also extremely useful to detect subtle changes in the proximal suspensory ligament that may not be visible or conclusive with ultrasonography. In addition, MRI allows accurate examination of the osseous structures adjacent to the suspensory ligament (metacarpal bones and distal carpal bones).
In contrast to hindlimb PSD, most horses with acute forelimb PSD respond well to rest and a controlled exercise program for 3–6 mo (~90% return to function). Premature return to work typically results in recurrence/persistence of lameness. Horses with chronic PSD may require a longer rehabilitation program or adjunct therapy (NSAIDs, shockwave, regenerative therapies) to return to consistent work.
Desmitis of the Body of the Suspensory Ligament:
This is principally an injury of racehorses. Injuries usually affect the forelimbs of Thoroughbreds and the forelimbs and hindlimbs in Standardbreds. Soreness on palpation of the forelimb suspensory ligament is quite common in horses with lameness associated with a more distal limb problem; however, structural abnormality of the ligaments is only rarely identifiable ultrasonographically. Clinical signs vary and involve enlargement of the ligament, local heat, swelling, and pain. Diagnosis is usually based on clinical signs and can be confirmed ultrasonographically. Treatment is aimed at reducing inflammation by systemic NSAIDs, hydrotherapy, and controlled exercise. Shockwave therapy, platelet-rich plasma, and stem-cell therapy have also been used for suspensory body lesions.
Desmitis of the Branches of the Suspensory Ligament:
This relatively common injury is seen in all types of horses in forelimbs and hindlimbs. Usually only a single branch in a single limb is affected, although both branches may be affected, especially in hindlimbs. Foot imbalance is often recognized in affected horses, and this may be a predisposing factor.
Clinical signs depend on the degree of damage and the chronicity of the lesion(s) and include localized heat and swelling. Swelling is often due to local edema of the affected branch. Effusion can be present in the adjacent palmar/plantar fetlock joint and/or the digital flexor tendon sheath. Pain is usually elicited either by direct pressure applied to the injured branch or by flexion of the fetlock. Lameness is variable and may be absent.
Courtesy of Dr. Matthew T. Brokken.
Diagnosis is based on clinical signs and ultrasonographic examination. Radiographic examination should also be performed to evaluate the attachment of the suspensory branch on the proximal sesamoid bones. Low 4-point diagnostic analgesia as well as intra-articular analgesia of the fetlock joint (varying degrees based on the location of the branch injury) improves lameness. Ultrasonography can detect a range of abnormalities, including enlargement, alteration of shape, and alterations in echodensity.
Management depends on the severity of the signs and on the breed and use of the horse. Shockwave therapy, local anti-inflammatories, ligament splitting, and regenerative therapy have all been used with varying results. Strict attention to foot balance is also critical in management of these lesions. Clinical signs may take ≥6 mo to improve, and the condition may recur. Prognosis for reinjury or persistence of lameness is worse in horses that are hyperextended in their fetlocks at rest or in horses with marked periligamentous fibrosis around the branch on ultrasound.